Trigger Point Injection therapy-
the what, where, how and why
Muscles are made up of countless fibers, all trying to work together, orchestrated contracting and relaxing so that we can move about our daily lives. But there is a lot of ways that the normal motion can get derailed.
Trigger points are areas of muscle, sometimes microscopic or sometimes the size of a cherry tomato, where the muscle fibers have been irritated and respond by developing local inflammation and shortening of those fibers. They can also develop in ligaments (connective tissue between bones) and tendons (connective tissue between muscles and bones).
These cause pain, tenderness and even 'nervy' symptoms such as numbness, pins and needles or sharp, shooting pains (see diagram below). The rotten thing is that because our body is very inter-connected, sometimes the pain is localized (hurts right where you press), but often with trigger points the pain travels to another area of the body (called radiating pain).
Trigger points are areas of muscle, sometimes microscopic or sometimes the size of a cherry tomato, where the muscle fibers have been irritated and respond by developing local inflammation and shortening of those fibers. They can also develop in ligaments (connective tissue between bones) and tendons (connective tissue between muscles and bones).
These cause pain, tenderness and even 'nervy' symptoms such as numbness, pins and needles or sharp, shooting pains (see diagram below). The rotten thing is that because our body is very inter-connected, sometimes the pain is localized (hurts right where you press), but often with trigger points the pain travels to another area of the body (called radiating pain).
These trigger points often accompany and may be factors underlying chronic conditions such as headaches, migraines, neck pain, shoulder pain and low back pain (image below shows most common locations). Trigger is in their very name. They trigger us.
They often trigger the development and worsening of conditions related to muscle pain. They can develop in any muscles, big or small. It doesn't matter if you are physically active or a couch potato, we are all susceptible to developing them.
They often trigger the development and worsening of conditions related to muscle pain. They can develop in any muscles, big or small. It doesn't matter if you are physically active or a couch potato, we are all susceptible to developing them.
What can be done?
Well, as a Naturopathic Doctor I am wanting to not only help get you out of pain, but investigate and try to determine why the trigger point developed. Is it due to posture? Abnormal muscle firing? Lack of restorative sleep or excess stress? A past injury or surgery? Another medical condition (such as autoimmune or neurological disease) or excess inflammation? To get long-lasting results, we need to understand and work to resolve all underlying reasons.
How do we get rid of trigger points?
There are many treatments offered, such as hands-on manual therapies offered by a Naturopathic Doctor, Chiropractic Doctor or massage therapist. These can often be very effective, though may need frequent or repeat in-office appointments.
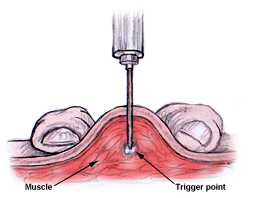
Trigger point injections (TPI) are offered by some doctors, including specially trained Naturopathic Doctors. If needles are used without injecting any solution (liquid), that is called 'dry needling'. Often with TPI, numbing solutions are used for maximal benefit.
What do TPIs do?
We can pin-point the problem area, turn off any abnormal nerve signaling and muscle firing, promote a healing response in that exact part of the body and immediately reduce inflammation, all with a quick injection to the very center of that trigger point.
What to expect from a TPI appointment?
Similar to a vaccination or a B12 injection, TPIs are quick injections into the muscle layer of the body (beneath the skin and fat layer). Just like vaccinations, the area is cleaned and at most a simple band-aid covers the site (often not even that is needed). See this video for a quick overview.
Well, as a Naturopathic Doctor I am wanting to not only help get you out of pain, but investigate and try to determine why the trigger point developed. Is it due to posture? Abnormal muscle firing? Lack of restorative sleep or excess stress? A past injury or surgery? Another medical condition (such as autoimmune or neurological disease) or excess inflammation? To get long-lasting results, we need to understand and work to resolve all underlying reasons.
How do we get rid of trigger points?
There are many treatments offered, such as hands-on manual therapies offered by a Naturopathic Doctor, Chiropractic Doctor or massage therapist. These can often be very effective, though may need frequent or repeat in-office appointments.
Trigger point injections (TPI) are offered by some doctors, including specially trained Naturopathic Doctors. If needles are used without injecting any solution (liquid), that is called 'dry needling'. Often with TPI, numbing solutions are used for maximal benefit.
What do TPIs do?
We can pin-point the problem area, turn off any abnormal nerve signaling and muscle firing, promote a healing response in that exact part of the body and immediately reduce inflammation, all with a quick injection to the very center of that trigger point.
What to expect from a TPI appointment?
Similar to a vaccination or a B12 injection, TPIs are quick injections into the muscle layer of the body (beneath the skin and fat layer). Just like vaccinations, the area is cleaned and at most a simple band-aid covers the site (often not even that is needed). See this video for a quick overview.
Depending on the size, area and extent of trigger points, sometimes just one appointment is needed. For more involved conditions, a short series or occasional repeat of TPIs gets us the most benefit. Often there is more than one trigger point present and problematic. Multiple trigger points can be addressed in one appointment, even if they are in different muscles, or also in ligaments and tendons.
If you have chronic, nagging muscle tightness, soreness, pain and radiating symptoms, then you may benefit from TPI. Call for an appointment with Dr. Angela, and get ahead of the pain-tightness-pain cycle that can often leave trigger points indefinitely trapped in our muscles.
Further resources and research
1. Imamura ST, Fischer AA, Imamura M, Teixeira MJ, Tchia Yeng Lin, Kaziyama HS, et al. Pain management using myofascial approach when other treatment failed. Phys Med Rehabil Clin North Am. 1997;8:179–96.
2. Cole TM, Edgerton VR. Musculoskeletal disorders. In: Cole TM, Edgerton VR, eds. Report of the Task Force on Medical Rehabilitation Research: June 28–29, 1990, Hunt Valley Inn, Hunt Valley, Md. Bethesda: National Institutes of Health, 1990:61–70.
3. Hong CZ, Hsueh TC. Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil. 1996;77:1161–6.
4. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:5.
5. Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22:89–101.
6. Ling FW, Slocumb JC. Use of trigger point injections in chronic pelvic pain. Obstet Gynecol Clin North Am. 1993;20:809–15.
7. Mense S, Schmit RF. Muscle pain: which receptors are responsible for the transmission of noxious stimuli? In: Rose FC, ed. Physiological aspects of clinical neurology. Oxford: Blackwell Scientific Publications, 1977:265–78.
8. Hopwood MB, Abram SE. Factors associated with failure of trigger point injections. Clin J Pain. 1994;10:227–34.
9. Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615–23.
10. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:94–173.
11. Rachlin ES. Trigger points. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:145–57.
12. Fischer AA. Injection techniques in the management of local pain. J Back Musculoskeletal Rehabil. 1996;7:107–17.
13. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:11–93.
14. Yunus MB. Fibromyalgia syndrome and myofascial pain syndrome: clinical features, laboratory tests, diagnosis, and pathophysiologic mechanisms. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:3–29.
15. Sola AE, Bonica JJ. Myofascial pain syndromes. In: Bonica JJ, ed. The management of pain. 2d ed. Philadelphia: Lea & Febiger, 1990:352–67.
16. Rachlin ES. History and physical examination for regional myofascial pain syndrome. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:159–72.
17. Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73:256–63.
18. Ruoff GE. Technique of trigger point injection. In: Pfenninger JL, Fowler GC, eds. Procedures for primary care physicians. St. Louis: Mosby, 1994:164–7.
19. Fischer AA. New approaches in treatment of myofascial pain. Phys Med Rehabil Clin North Am. 1997;8:153–69.
20. Zohn DA, Mennell JM. Musculoskeletal pain: diagnosis and physical treatment. Boston: Little, Brown, 1976:126–9,190–3.
If you have chronic, nagging muscle tightness, soreness, pain and radiating symptoms, then you may benefit from TPI. Call for an appointment with Dr. Angela, and get ahead of the pain-tightness-pain cycle that can often leave trigger points indefinitely trapped in our muscles.
Further resources and research
1. Imamura ST, Fischer AA, Imamura M, Teixeira MJ, Tchia Yeng Lin, Kaziyama HS, et al. Pain management using myofascial approach when other treatment failed. Phys Med Rehabil Clin North Am. 1997;8:179–96.
2. Cole TM, Edgerton VR. Musculoskeletal disorders. In: Cole TM, Edgerton VR, eds. Report of the Task Force on Medical Rehabilitation Research: June 28–29, 1990, Hunt Valley Inn, Hunt Valley, Md. Bethesda: National Institutes of Health, 1990:61–70.
3. Hong CZ, Hsueh TC. Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil. 1996;77:1161–6.
4. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:5.
5. Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22:89–101.
6. Ling FW, Slocumb JC. Use of trigger point injections in chronic pelvic pain. Obstet Gynecol Clin North Am. 1993;20:809–15.
7. Mense S, Schmit RF. Muscle pain: which receptors are responsible for the transmission of noxious stimuli? In: Rose FC, ed. Physiological aspects of clinical neurology. Oxford: Blackwell Scientific Publications, 1977:265–78.
8. Hopwood MB, Abram SE. Factors associated with failure of trigger point injections. Clin J Pain. 1994;10:227–34.
9. Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60:615–23.
10. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:94–173.
11. Rachlin ES. Trigger points. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:145–57.
12. Fischer AA. Injection techniques in the management of local pain. J Back Musculoskeletal Rehabil. 1996;7:107–17.
13. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial pain and dysfunction: the trigger point manual. 2d ed. Baltimore: Williams & Wilkins, 1999:11–93.
14. Yunus MB. Fibromyalgia syndrome and myofascial pain syndrome: clinical features, laboratory tests, diagnosis, and pathophysiologic mechanisms. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:3–29.
15. Sola AE, Bonica JJ. Myofascial pain syndromes. In: Bonica JJ, ed. The management of pain. 2d ed. Philadelphia: Lea & Febiger, 1990:352–67.
16. Rachlin ES. History and physical examination for regional myofascial pain syndrome. In: Rachlin ES, ed. Myofascial pain and fibromyalgia: trigger point management. St. Louis: Mosby, 1994:159–72.
17. Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil. 1994;73:256–63.
18. Ruoff GE. Technique of trigger point injection. In: Pfenninger JL, Fowler GC, eds. Procedures for primary care physicians. St. Louis: Mosby, 1994:164–7.
19. Fischer AA. New approaches in treatment of myofascial pain. Phys Med Rehabil Clin North Am. 1997;8:153–69.
20. Zohn DA, Mennell JM. Musculoskeletal pain: diagnosis and physical treatment. Boston: Little, Brown, 1976:126–9,190–3.