|
A message from my clinic, Reconstructed Wellness, on Juneteenth:
The eve of January 1st, 1863, also known as “Freedom’s Eve”, at midnight the Emancipation Proclamation took effect and all enslaved people in the confederate state were declared free. This declaration was not immediately recognized, and it wasn’t until June 19th, 1865, that Union soldiers came to Galveston Bay Texas to announce that the enslaved people in that state were free by executive order. If you are white, of European descent, or feel this is your business to attend to, please consider taking this day to educate yourself, donate, support, and make reparations. Let us reflect on the ways our government and culture are still entrenched in these root oppressive systems and continue to be racist and harmful—the ways we are part of this history, and the ways we participate in and benefit from these systems. Below please find some resources for donations, reparations, and education. Brown Hope https://brownhope.us18.list-manage.com/track/clicku=81934e15afd2f4fad57d7c60b&id=cc890cdc6e&e=a07138f027 Don’t Shoot PDX https://www.dontshootpdx.org/ Leilani Foundation https://theleilanifoundation.org/ Anti racist work for white people: https://surj.org/ Black owned businesses in Portland https://mercatuspdx.com/directory/black-owned-businesses/#!directory/ord=rnd Possible reading https://www.theroot.com/make-juneteenth-great-again-the-caucasians-guide-to-ce-1847124121
0 Comments
It is no secret that physician burnout is at an all time high. The following passages are taken from the article " Caring for oneself to care for others: physicians and their self-care" by Sandra Sanchez-Reilly, MD, MSc et al. (To read the full article CLICK HERE.) Clinicians who care for seriously ill patients face a high risk for diminished personal well-being, including burnout, moral distress, and compassion fatigue. Burnout is defined as a “progressive loss of idealism, energy, and purpose experienced by people in the helping professions as a result of the conditions of their work.” It is further defined by 3 key characteristics:
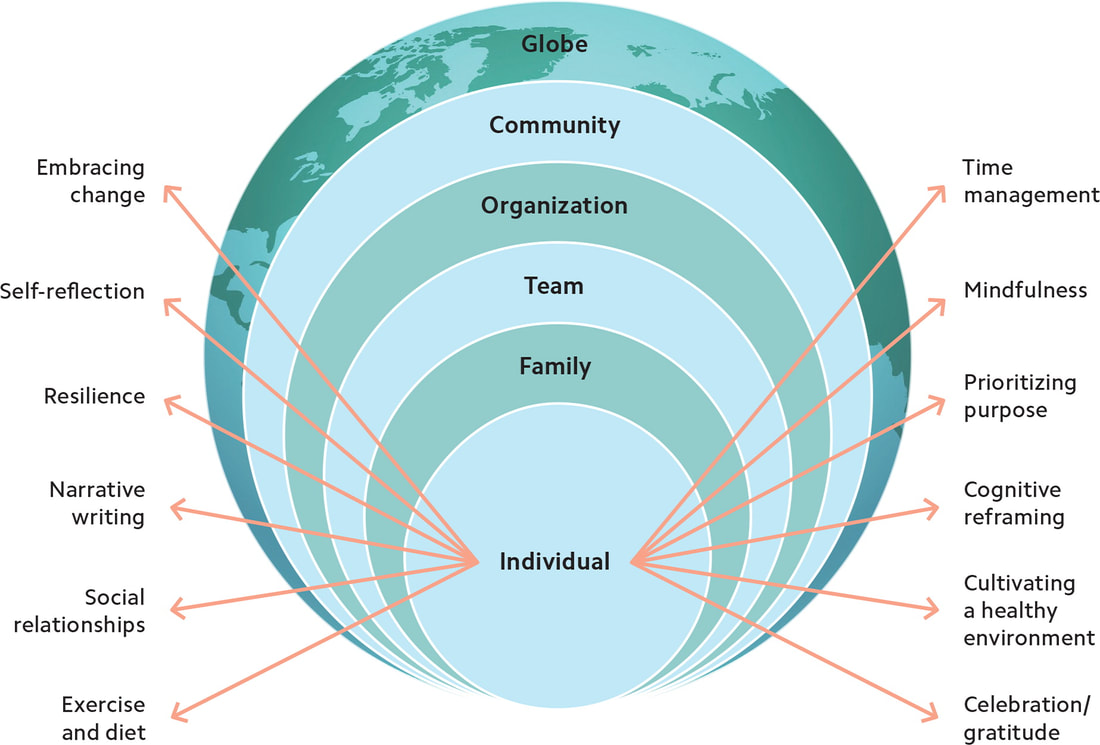
All physicians can be at risk for burnout as a result of both work and personal characteristics. Work factors include work overload (eg, large patient volumes, insufficient resources, or feeling poorly managed), lack of control over one's work environment, having the bulk of one's time at work spent on tasks inconsistent with one's career goals, and high levels of work-home interference. The consequences of burnout, compassion fatigue, and moral distress are profound and range from personal crisis to suboptimal patient care practices. Given the inadequacy of self-care education for physicians, we must ask how these physicians can be better equipped to face the stresses inherent in the work. Improving physicians' wellness and implementing self-care strategies is a multifactorial process and includes attention to both personal and professional self-care. Some key strategies to mitigate stress and burnout and promote well-being include:
It is for these exact reasons (and many more!) that I have created my Restorative Embodiment Retreat. Please consider joining me in Tuscany in October 2025. You can find full retreat details HERE.
Take good care of yourself. You are worth it! Dr. Angela The following is an excerpt from "Caring for Me Is Caring for You: The Power of Physician Self-Care and Personal Transformation" by Catherine Florio Pipas, MD, MPH: " 'One A Day' is a multivitamin designed to promote good health. It also represents the approximate number of physicians who die by suicide daily in the United States. Even one preventable death is too many, and it is a tragedy that as health professionals we are often not able to care for ourselves as well as we care for our patients. Many stressors contribute to the rising cycle of burnout, depression, and suicide among health professionals. Chronic stress that results from workload exceeding workforce, lack of time and control, and feelings of inadequacy and hopelessness are just a few of the causes. The stigma around mental health and self-care often limits professionals from seeking help or even acknowledging they need a break. Additionally, despite having the knowledge and skills to diagnose and treat others, physicians do not effectively recognize burnout in themselves." Let's sit with that for a minute. One physician per day dies by suicide in the United States alone. Physicians do not effectively recognize burnout in themselves. It's clear that changes need to be made. But where do we start? Dr. Florio Pipas suggests that the best place to start is with ourselves. Some key points from her article include the following:
She encourages us to use The Social Ecological Model which "illustrates how change begins with each of us as individuals applying a variety of wellness strategies, and then it spreads outward to our families, teams, organizations, communities, and beyond." I strongly share this belief, which is why I created my Restorative Embodiment Retreat. It is designed to be a week away from the demands of daily life and work to refocus on ourselves as individuals and get back into balance. Please consider joining me. (Click here for full retreat details.) I would also encourage you to read the full article --->here<--- Have a good week! Take care of yourselves, and each other. Dr. Angela "According to the American Counseling Association (ACA), secondhand, or vicarious, trauma is a condition that affects many people who interact with those who have experienced a traumatic event. When those in helping professions hear clients talk about what they experienced and see their physical reaction to the experiences, they may also begin to feel the effects of trauma. In some cases, the condition can be a cumulative effect from hearing multiple accounts in their daily work... Unchecked, secondhand trauma can be debilitating, like the emotional numbing associated with compassion fatigue. When those in helping professions see a great demand for their services, they may ignore signs of their own trauma to serve others." (You can read the full article titled "Resource Guide for Coping with Secondhand Trauma" here. I would encourage you to do so- it's full of many important resources!) I created my Restorative Embodiment retreat to serve as an important way to combat the many effects of Secondhand Trauma. What this retreat is:
--->Full retreat details here!<--- I hope you can join me! Please join me this Sunday, April 7th at 10:00am PST for a live Zoom Q&A where I will be available (in addition to our facility host) to answer all of your questions about my upcoming Restorative Embodiment Retreat!
This retreat is an intentional dedication of our time and attention to address that which is working against us in our daily life, peeling back the layers of stuck-ness us busy professionals tend to impressively accumulate. (This photo is just one of the many gorgeous Tuscan views we will be enjoying.) You don't want to miss it! Zoom invitation: Topic: Restorative Embodiment Retreat Q&A Session Time: Apr 7, 2024 10:00 AM Pacific Time (US and Canada) Join Zoom Meeting https://us05web.zoom.us/j/87677335895?pwd=KSpbBaGTwLbO9ihcGRzNaHxageltln.1 Meeting ID: 876 7733 5895 Passcode: RbXmr8 More details about my retreat can be found ------> Here<------- A recent study conducted in Greece found that Secondary Traumatic Stress (STS) is on the rise in healthcare workers. It also concluded that “Secondary Traumatic Stress is an aspect of “cost of care”, the natural consequence of providing care to people who suffer physically or psychologically.”
But is it though? Or is it a natural consequence of under-resourced healthcare providers working in an unjust system with lack of support? I would argue that the latter is true. We shouldn't have to accept stress, trauma, and burnout as a natural consequence of working in our chosen field. If you're feeling the effects of Secondary Traumatic Stress, please consider joining me for a week in Tuscany to combat the burnout. You can find the full retreat details here, and a link to the above-referenced study here. It is no secret that the stress of dealing with a pandemic over the past 4 years has "heavily impacted the psychological and emotional wellbeing of the general population and healthcare workers". (Full study data can be found ---> here.)
Burnout, Secondary Traumatic Stress, Secondhand Trauma, Vicarious Trauma, and Compassion Fatigue are all the same, and everyone is suffering. The most common symptoms in healthcare workers are emotional exhaustion (56%) and depersonalization (48.9%), and it is no surprise that physician burnout is on the rise. You deserve better. We ALL deserve better. Please join me for a week of RE-personalization where you can focus on your own needs and getting back into balance. Details are only -->one click<-- away. "Almost all physicians regularly experience burnout and more than half have considered leaving or no longer seeing patients, a survey found.
A total of 93% of approximately 1,000 physicians surveyed online -- three-fourths of whom were primary care doctors -- said they feel burned out regularly; they also reported working an average of 15 hours per week outside their regular workday." This excerpt is from an article titled “How Many Docs Are Feeling Burned Out?” by Joyce Frieden. (Spoiler alert- it’s nearly all of them.) You can read the full article ----> here. Nearly half of those polled (49%) said their daily workload is unsustainable. 77% said they felt overwhelmed by excessive communication demands such as feeling that they were "expected to respond to patient communications at "all hours of the day, every day of the week." It is for these reasons (and many more!) that I created my Restorative Embodiment retreat. Join me in Tuscany for an all inclusive week focused on prevention of practitioner burnout. --> Click here <-- for more info! As we're continuing into the holiday season, I wanted to share a few more office updates and plans I'm looking forward to. New services for migraines and neuropathyI have recently shared a few new additions to my practice:
Because I am always learning more, in order to best help my patients, I will soon be offering a few more new services: Botox injections for migrainesNow, I'm not an esthetic (medi-spa) practitioner. I like your grey hair and wrinkles. AND, the current migraine treatments available are often... lacking. Even doing my best to help migraines using Naturopathic therapeutics, medications, well.... migraine meds often just suck. It is often hard for someone experiencing migraines to find a migraine med that works well, that doesn't knock them out with side effects. So, introducing: botox injections. Now, this is nothing new. The FDA approved the use of botox injections for migraines back in 2010. And in the Portland area, historically I have had a few neurologists who I could refer to for this service. But (as those of you who also live in Salem may know), when I'm looking for a specialty service like this in Salem... it's often nowhere to be found. I joke that Salem is a really big small town. But when it comes to the unavailability of specialized care, that's just no joke for any of us. Since I know just about every other injection procedure under the sun, my training on this will be very fast. I'll be learning from some injection instructors in Arizona next month, and I'll be able to start offering this service starting January at the latest. Small fiber neuropathy - further evaluation now available in SalemSmall fiber neuropathy (SFN) appears to be more common among those who have Ehlers-Danlos syndrome, Mast Cell Activation Syndrome, Postural Orthostatic Tachycardia Syndrome (POTS), Lupus, other autoimmune diseases, Fibromyalgia, other rheumatic diseases, Interstitial Cystitis and other chronic, complex conditions. While this announcement is perhaps not relevant for many of my patients, an increasing number do have one or more of the above conditions, so I didn't want anyone to miss out on finding out about this. So again, just because I got fed up with not being able to find anyone in Salem who can work up my patients for small fiber neuropathy (SFN), I will start offering biopsy evaluation for this concern at both of my clinics. Dr. Menk Otto (who also practices at my Portland location), has been offering these for a little while, as do a few others I know of in Portland. But in Salem... it's been... just crickets. For those who are curious, SFN is a condition that affects the nerves, usually starting in the skin of the hands and/or feet. Someone may have neuropathy (nerve pain and/or sensory changes) due to a known condition (such as diabetes), temporary deficiency (hypothyroidism, low vitamin B12 or copper) or a past injury. If the reason for the neuropathy is not known, sometimes this condition needs to be evaluated. The best way to evaluate this condition is with a skin biopsy, comparing the number, shape, and density of nerves in the upper and lower legs. I will still be referring out patients for biopsies for other conditions (such as uterine or skin conditions), I am not trying to be the expert in all things for all people. But for this specific condition, it has been difficult to find experts to refer out for in the Salem area. This too will be available starting in January. If this is a concern for you (maybe we've tried and failed to find a local practitioner to do this biopsy?), then first things first is an in-office evaluation focusing on a neurologic workup. Then, if we decide to go forward with the biopsy, that visit must happen in the morning (due to the very specific nature of the biopsy procedure and the very particular way that it needs to be shipped). Further reading: About SFN: https://www.hopkinsmedicine.org/neurology-neurosurgery/specialty-areas/peripheral-nerve/small-fiber-sensory-neuropathy https://www.medicalnewstoday.com/articles/small-fiber-neuropathy#causes Scientific articles on SFN: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3086960/ And on that note, just two more little bits of news… additional care, outside of office visitsI try not to be too much of a Luddite when it comes to technology. But also, I was trained in the paper chart era. In-office visits with paper charts, having staff return phone call messages, that was the extent of my medical training as it pertained to avenues of delivering care. So while I have known about these "online digital evaluation and management" service codes for a year or two, I just didn't know how they would benefit my patients, nor how they could get integrated into the care I offer. As more and more systems are digital, and many care basics can and are handled before and after visits, these digital care codes are starting to make more sense. There are three codes (99421, 99422, 99423) and they indicate 5-10 minutes, 11-20 minutes, and more than 20 minutes respectively. Here are a few examples of where I can handle some aspects of care outside of an office visit, so where these codes may be used in place of a visit:
These codes are definitely no replacement for face-to-face care, whether that is in-person or via telehealth. This type of care is limited to what I can do on my own, essentially without having a conversation with you. If I need to ask you questions, discuss treatment alternatives, side effects, etc. - conversations still need to happen within visits. And, no matter how well things are going, and how good you feel, the management of many prescriptions still requires 1-2 visits per year (no matter what our opinions may be on the matter), along with whatever lab evaluation is standard to that management. This may open the door to patients getting a few straight-forward needs met between their visits. So if you may find this helpful, you can check with your insurance as to coverage for those codes. I am not punctualHi, my name's Angela, and I am running behind on visits most of the time. I apologize. I actually used to be very punctual. No, really! Back when insurers paid for longer visits, the visit times were scheduled longer. I was known for my punctuality and even started visits early when I could. Now, they don't cover that time. So we don't schedule for that length of visits. Add to that a new dynamic in my practice... The depth and complexity of what I can evaluate and treat for patients has exponentially developed over the last 5 or so years. I used to refer out for many chronic, complex conditions that I am now known as being the go-to expert. Well, the expert in Salem. There are still many great experts in the Portland area (though they may be scheduling far out for new patient visits, not taking new patients right now, or have dropped all insurance contracts - it's strange being in the medical field right now). A few of those conditions are those I mentioned above, such as Ehlers-Danlos syndrome (I'm most experienced with hEDS), Mast cell activation syndrome, Postural orthostatic tachycardia syndrome (POTS), Fibromyalgia, autoimmune, neurologic, rheumatic and other chronic, complex conditions. You know, the kind of conditions and concerns that when you bring them up, the typical "5 minutes and I'm out" provider gets wide-eyed, panicked, and starts looking for the door. I'm over here, leaning in, asking you to speak more about it. That's my style, and that's how I figure out where we can go next. And, in all my excitement to discuss new tests, treatments, and options my patient has often never heard of (the patient who had practically given up all hope), my timing starts to fall really, really behind. I do apologize. I do recognize being punctual is a form of respect. But in the course of respecting patients with really tricky, complex conditions, I end up disrespecting the timing of the patient who comes afterward. I get that. And I feel stuck. Because I can't cut patients off after their first 1-3 symptoms like other clinics who literally post this policy at the reception desk. I just don't do medicine that way. So, if you want me at my most timely, ask for the first appointment of the day (or the first appointment after my lunch break). It is extremely rare that I start my appointments late from the get-go. It's just that I fall behind providing the care I want to deliver within the confines that insurers place on my practice. One new thing I'm bringing into my clinic to help with my timeliness is digital transcription. I am going to start using a program that helps me chart. The program will be listening, but it's a HIPAA-compliant computer program, not a person. It then helps with my notes, and only those notes are kept. No recording. So, no one will be listening, and no recording will be stored anywhere. And also, this program is separated from the private, identifying information we keep on patients, so none of that is associated with my dictation. And although in my trials I have seen how it will help in the efficacy of my charting and creating treatment plans for patients, I also realize that new technology like this will not be desired by all. If you wish for me to not use this during our visits, please just ask (though I really hope the patients who do ask this don't also have Alexa, Facebook app, or any other number of tech gadgets listening to you in order to sell you things if you ask for this level of tech privacy). dang it, and I thought this would be a short oneI am just wordy. There's no helping it.
I hope you are staying warm during our transition to winter. I'm going to try to take a little downtime this week, with some hot tea, blankets and a good book. Take care for now, and I hope you also find some relaxing quality time this week, Dr. Angela Cortal As we're saying goodbye to October and hello to November, I would like to share a couple of current office updates and future plans. an update on phone numbersFor some reason, about a month ago my schedule got very chaotic with patients being scheduled at the wrong clinic (ex: they wanted to see me in Salem, but ended up on my Portland schedule). Now I've known this could happen, since I work at two separate locations under one practice name, but it's never been too much of an issue before. I believe now staff are confirming location a little bit more during phone calls ("for the Salem office, you're wanting to see her at the Salem office, right?"), so it looks like everything has smoothed out. But just in case you don't have both phone numbers, here they are: Portland: 503-232-3215 Salem: 503-990-8395 We were considering "closing down" the schedules at the respective clinics (Portland staff would only be able to schedule me for my Portland schedule), but it seems like the chaos has calmed down. In any case, please at least save into your phone the number for the office you physically see me at, and call that one when you're scheduling follow-ups. updates around the officeSome days I will have a colleague or medical intern shadowing me. For the most part they are all looking to further develop their injection therapy skills, or exposing themselves to this field in order to learn more about it (and decide whether to pursue it post-graduation). I strive to respect everyone's needs and boundaries, so during the days I have someone in the office with me, I do a quick check with each patient as soon as they get here (for injection procedure and/or re-evaluation follow-ups post-injections). I check in to see whether they are comfortable having someone observe the entire visit, just the injection procedure component, or not at all. That way there are no surprise visitors during visits, and my colleagues/ students get observation experience with those who feel comfortable with them being present. a few more office updatesAlpha Stim I have been doing a lot of research into different in-office electrotherapy devices, such as cranial electrotherapy stimulation (CES), transcranial magnetic stimulation (TMS), and vagus nerve stimulation devices. After a lot of careful consideration, I have decided to offer Alpha Stim at both of my clinics.This is a CES device that is FDA-cleared for anxiety, insomnia and pain. I will start offering these 30-minute sessions during office visits (you can schedule a typical in-office follow up for this). When treating anxiety, depression, or insomnia, those sessions can be billed to insurance (limit: 4 sessions). That way I can offer a more approachable trial run for this device to my patients, and those who benefit can decide whether to obtain one from my office or the Alpha Stim company for at-home use. Ketamine I have been following the research and medical use of ketamine for the last few years with a lot of interest. As this field develops, we are seeing more evidence-based uses of ketamine for pain, insomnia, anxiety, and depression. I am often brainstorming with patients more and different options after chronic pain management or conventional mental health treatment of therapy and pharmaceuticals have been exhausted. There is of course no one magic bullet for any of these complex chronic concerns, but I am interested in learning more about it, as it could be one more additional treatment option I can offer my patients. I will only be offering oral options, which should be used in conjunction with ongoing mental health counseling. I will not be offering it IV. Here are a few articles on some of the medical uses of ketamine, if you are interested in learning more: https://www.medrxiv.org/content/10.1101/2020.07.13.20153247v2.full https://www.nature.com/articles/s41398-021-01230-z https://www.psychiatrist.com/jcp/oral-ketamine-for-depression/ In order to prescribe ketamine I have to take additional continuing education and certification. So, I don't have that yet, but I expect towards the end of the year, or the beginning of 2024, this will be one more treatment I can offer patients. a note on billing codes, and when more than one code is used for one visitIf your visits with me are not billed to your insurance plan, you can just go ahead and skip this fairly dry subject. For the rest of you, I wanted to take a moment to describe how and when I use what codes. I hope that no one's eyes glaze over in boredom, but I feel that I'm the best to discuss this subject because when insurance billing questions come up, it is usually our office manager Iris who handles this. And Iris is great, we all love Iris, however she is not present during the visits, so she just has to guess why and how I'm using the various codes that I do. A common category is called an extended time code. The best way I can describe this, is think back to the last visit you had with a "standard" medical provider for your concern (pain, hormones, diabetes, thyroid, GI, you name it). How long was that visit? How many other conditions did you discuss and make a plan for that day? If your provider was following typical norms, the average appointment time is 5-7 minutes, and is focused just on that one concern. If you bring up another concern, the provider often will tell you that you have to book a separate visit to address that second concern. Now compare that to a typical office visit with me, which lasts 30-60 minutes. I am often working up many concerns at once (your chronic joint pain, your allergies, your hormone deficiency, reviewing your blood sugar labs, and what is this weird new thing on my skin???). With how codes are set up, I'm not going to bill four office visit codes just because I cover four of your concerns (and that's a very low estimate for what's typical in my visits). Instead, I will bill an office visit code with an extended time code. The first code tells your insurance company we had a medical visit. The second code tells them we went into a lot of depth above and beyond typical office visits. Other types of codes I use, in addition to office visit codes, are:
ok, that's enough updates for nowI hope you have a lovely fall, and can enjoy our entry to the cozy, warm, hibernation season. I've been enjoying breaking out my herbal tea blends again, and snuggling up under blankets with a good book.
I wish you the very best in feasting, friends, family, loved ones, or any other seasonal quality time you enjoy, Dr. Angela Cortal |
Archives
June 2024
Categories
All
|
about the doc |
patient infocontact |
|
Privacy Policy
© Copyright 2011-2024, Dr. Angela Cortal ND LLC website content is for educational purposes only and is no substitute for medical advice (see the Terms of Use Agreement for this site), you must establish a doctor-patient relationship to receive that! |